Abstract
BACKGROUND: HLH is a highly fatal hyperinflammatory disorder that mimics sepsis in adults. Diagnostic criteria have not been validated in adults and standards for therapy have not been established. As a result, delays in diagnosis are common. Elevations in temperature, ferritin, and soluble interleukin 2 receptor (SIL-2R) are associated with HLH. Based on the Agency for Healthcare Research and Quality (AHRQ) National Inpatient Sample data, the mean cost per hospitalization of adult patients with HLH in 2014 was $70,860 in 2017 US Dollars, with a mean length of stay (LOS) of 16.8 days. In contrast, mean cost per hospitalization in patients with severe sepsis was just $30,149, with a mean LOS of 8.1 days.
OBJECTIVE: To characterize inpatient resource requirements of adults with HLH as a benchmark for improvement in care and cost optimization.
METHODS: Adult HLH patients at Stanford Health Care (SHC) were identified using ICD9 code 288.4, ICD10 D76.1, D76.2 and associated keyword searches in the Epic electronic medical record and PowerPath pathology database. Clinical parameters associated with HLH diagnosis and management were identified by retrospective chart review and included: intervals between onset of symptoms, diagnosis, and therapy; labs, imaging, medications, underlying cause, infections, Sequential Organ Failure Assessment (SOFA) score for sepsis, transfusions, ward services, intensive care unit (ICU) services, palliative care consultation, and length of inpatient stay. An increase of SOFA score of ≥2 points defines organ dysfunction secondary to infection. Distribution of inpatient costs were used to extrapolate estimated costs based on the AHRQ-reported cost of $70,860. Costs were explored descriptively. Medians are reported when significant outliers were present.
RESULTS: Fifty nine adults (mean age of 52, SD土19.6 years) with 127 hospital encounters related to HLH were identified from January 2012 to May 2017. Thirty three (56%) had underlying malignancy (number, percentage): diffuse large B cell lymphoma (16, 48%), extranodal NK/T cell lymphoma nasal type (6, 18%), peripheral T cell lymphoma (4, 12%), other subtypes of T cell lymphoma (5, 15%), Hodgkin lymphoma (2, 6%), multiple myeloma with MDS (1, 3%), primary myelofibrosis (1, 3%), ovarian dysgerminoma (1, 3%). Thirteen (22%) patients had an underlying autoimmune disorder: systemic lupus erythematosus (4, 28%), rheumatoid arthritis (3, 21%), sarcoidosis (3, 14%), and dermatomyositis (3, 21%). Infections overlapped with other etiologies in 30 patients: EBV (22, 73%), CMV (4, 13%), HSV-1 (1, 3%), HHV6 (3, 9%), HHV8 (1, 3%), mycobacterium avium (1, 3%), and histoplasmosis (2, 6%). Other causes were: multiple viruses (2, 3%), left ventricular assist device (4, 7%), pregnancy (1, 2%), primary (2, 3%), allogeneic stem cell transplant (allo SCT), (2, 3%), idiopathic (4, 7%). Blood products transfused in units (SD): red cells: mean 7, median 4 (土5); platelets: mean 7, median 2 (土7); plasma: mean 2, median 0 (土2); cryoprecipitate: mean 2, median 0 (土2.5). Mean LOS (土SD) in days was 16 (土20), with 4 (土11.5) days in the ICU. For transferred patients (25, 42%), outside hospital LOS was an additional 10 (土16) days.
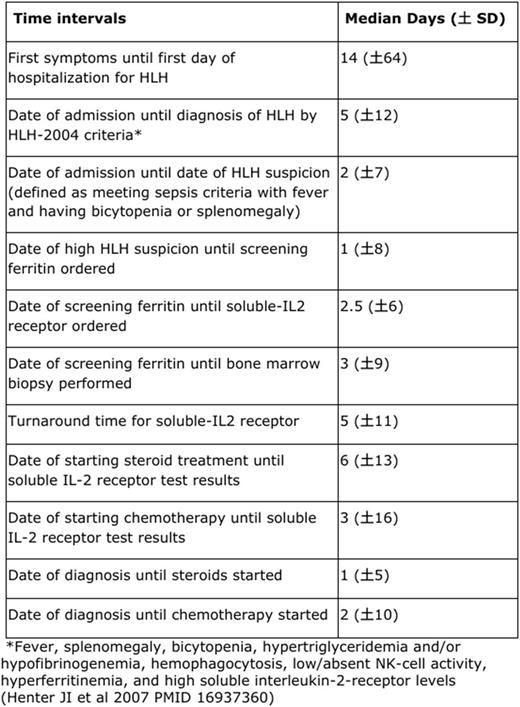
The mean distribution of costs relative to AHRQ data were: ICU services: $12,828; medications: $12,771; ward services: $8,468; laboratory studies: $7,254; blood products: $4,865; imaging: $1,393. Costs of the first hospitalization were 128% (p<0.001) higher than later hospitalizations. Table 1 describes the median (土SD) difference in days from clinically important endpoints across all patients. An increase in SOFA score of at least 2 from baseline to the date of suspicion HLH occurred in 92% of cases, with a median increase of 4土4 SOFA points. Thirty-three (55%) patients died, 25 from HLH, in whom median time from symptoms to diagnosis was 18 (土93) days, and survivorship after diagnosis, 30 days (土57). Palliative care was consulted in 44% of patients who died from HLH. Allo SCT was performed in 4 (6%) patients at a median of 276 (土99) days from diagnosis.
Conclusion: Adult HLH is a heterogeneous, diagnostically perplexing hyperinflammatory disease with organ dysfunction resulting in elevated SOFA scores. High absolute and relative resource utilization, both in terms of cost of care and LOS, were evident.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal